Prior Hospitalizations Associated With Readmission with CDI
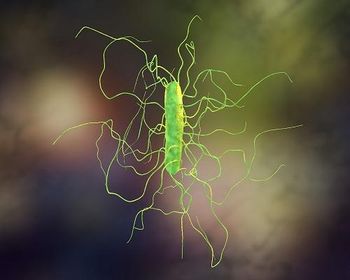
A third of patients hospitalized with community-onset Clostridioides difficile infections had recently been discharged from the same hospital, and most of those received antibiotics, according to research presented at IDWeek.
Prior hospitalizations may be a significant factor in readmission with community-onset Clostridioides difficile infections (CDI), according to a poster presentation at IDWeek.
The study reviewed data from the U.S. Centers for Disease Control and Prevention’s Emerging Infections Program, which identified 15,512 cases of C diff at 10 EIP sites in 2017. Among those for which medical records were obtained, 4,724 were hospitalized in 86 hospitals, including 2,984 (63.2%) that were identified as community-onset infections.
Common perception is that these are acquired outside of the hospital, but the investigators hypothesized that many of these infections were associated with previous hospitalizations and examined medical records to test their theory.
“A third of patients admitted with community-onset Clostridioides difficile infection had been recently discharged from the same hospital, and most had received antibiotics during or soon after the last admission,” presenter Alice Guh, MD, MPH, medical officer and the CDC’s lead for Clostridioides difficile infection surveillance. “This suggests that a substantial portion of hospitalized community-onset CDI might represent post-discharge cases associated with a previous hospital admission.”
Community-onset cases were placed in 4 categories depending on whether the patients were admitted from a long-term care facility (LTCF), a long-term acute care hospital (LTACH), a private residence but had a prior healthcare-facility admission within 12 weeks (CO-HCFA) or had no recent healthcare-facility admission (CA).
Among the 2,984 hospitalized community-onset cases:
• 1,424 (47.7%) were CA
• 1,201 (40.3%) were CO-HCFA
• 350 (11.7%) were LTCF-onset
• 9 (0.3%) were LTACH-onset.
Among those with a prior healthcare-facility admission (CO-HCFA), 1174 (97.8%) had a prior hospitalization, including 978 (83.3%) who were discharged from the same hospital, accounting for 32.8% of all the 2,984 hospitalized community-onset cases. Among those 978 recently discharged from the same hospital, 84.4% had received antibiotics during the prior 12 weeks.
These findings suggest that prior hospitalizations may have played a role in the development of CDI.
Limitations of the study include that it did not include data from non-catchment-area residents and incomplete medical records may underestimate recent exposure to antibiotics.
“Hospital-based and post-discharge interventions aimed at improving antibiotic use could potentially help reduce subsequent CDI hospitalizations,” Guh said. “More efforts are needed to identify effective interventions to prevent post-discharge CDI. This may include improving antibiotic prescribing at the time of discharge to help reduce inappropriate or excessive antibiotic use after the patient leaves the hospital.”
Efforts to control CDI are an ongoing focus. A
Another
Newsletter
Stay ahead of emerging infectious disease threats with expert insights and breaking research. Subscribe now to get updates delivered straight to your inbox.