Physicians Called on to Recognize and Report Monkeypox
Community transmission of monkeypox outside traditional endemic regions of the virus prompts calls for increased vigilance.
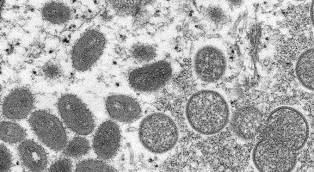
The apparent person-to-person spread of monkeypox outside of traditional African endemic regions of the virus, between persons who have not traveled to the regions or had contact with host animals, has prompted calls for increased vigilance and prompt reporting to public health.
A column in the Annals of Internal Medicine written on the occasion of the first confirmed case in the US, but published a few days later as the CDC just increased the confirmed case count to 9 in the US—and with more than 265 cases detected recently worldwide, calls on physicians in a range of practice settings to be alert to the presentation. At an IDSA media briefing on June 1, it was reported there was 18 cases in the United States and 600 worldwide.
"Containment efforts will rely on enhanced case finding, isolation, contact tracing and postexposure vaccination," say Amesh Adelja, MD, Johns Hopkins Center for Health Security, Baltimore MD and Tom Inglesby, MD, Johns Hopkins Bloomberg School of Public Health.
"Primary care physicians, urgent care physicians, emergency medicine physicians, dermatologists, and those working in STI [sexually transmitted infection] may be the most likely to identify new patients with monkeypox should they continue to appear," Adelja and Inglesby advised.
The authors note that monkeypox, in the orthopoxvirus family with smallpox, spreads through respiratory droplets, direct contact or fomites. Although airborne transmission is considered a theoretical risk by the CDC, they indicate that transmission from direct contact is more likely; that the incubation period can range from 5 to 21 days; and that a person is not contagious until symptoms begin.
CDC Director Rochelle Walensky emphasized that the risks for transmission "are not contained within social networks, and the risk of exposure is not limited to any one particular group."
Adelja and Inglesby recommend that clinicians should consider the possibility of monkeypox when encountering patients with new onset of febrile illness and rash, especially if accompanied by lymphadenopathy. A definitive diagnosis requires polymerase chain reaction (PCR) testing of skin lesions or fluid—available at state public health laboratories (there is no commercially available test currently).
Although there is no standard-of-care treatment, Adelja and Inglesby suggest smallpox antivirals with poxvirus activity, such as cidofovir, brincidofovir, and tecovirimet. (the latter 2 are approved by the FDA for smallpox treatment) could be obtained through a public health department or the CDC for severe cases or in immunocompromised persons.
Postexposure smallpox vaccine for contacts has been shown to limit transmission of monkeypox. Adelja and Inglesby indicate that administration immediately after possible exposure can abort the infection or significantly attenuate it. Although a newer generation vaccine, JYNNEOS, Bavarian Nordic, has FDA approval for prevention of monkeypox, they suggest that the older-generation ACAM2000 can also exert this preventative effect. In cases in which smallpox vaccine is contraindicated, Adelja and Inglesby indicate that vaccinia immune globulin can serve as an alternative postexposure prophylaxis agent.
Noting that the current outbreak is much larger and more widespread than prior monkeypox outbreaks outside of Africa, Adelja and Inglesby declare "the most pressing immediate challenge is to unravel the epidemiology of this outbreak."
Newsletter
Stay ahead of emerging infectious disease threats with expert insights and breaking research. Subscribe now to get updates delivered straight to your inbox.
