Ruptured Echinococcal Pulmonary Cyst
Here is a review of this specific case.
FINAL DIAGNOSIS
Ruptured echinococcal pulmonary cyst
HISTORY OF PRESENT ILLNESS
A man aged 29 years presented to the emergency department with progressively worsening right-sided chest pain of 1 week duration. His symptoms started 2 days after he underwent an outpatient bronchoscopy for a cystic mass found in his right lung. The chest pain was a pressure-like sensation that worsened with movement and deep breaths. He also had a productive cough with foul-smelling, dark-colored sputum; subjective fevers; and chills. Acetaminophen did not provide any relief.
MEDICAL HISTORY
Five years prior, he had an echinococcal liver cyst that was treated with a hepatic segmentectomy and a course of albendazole. He had no known lung lesions during that time.
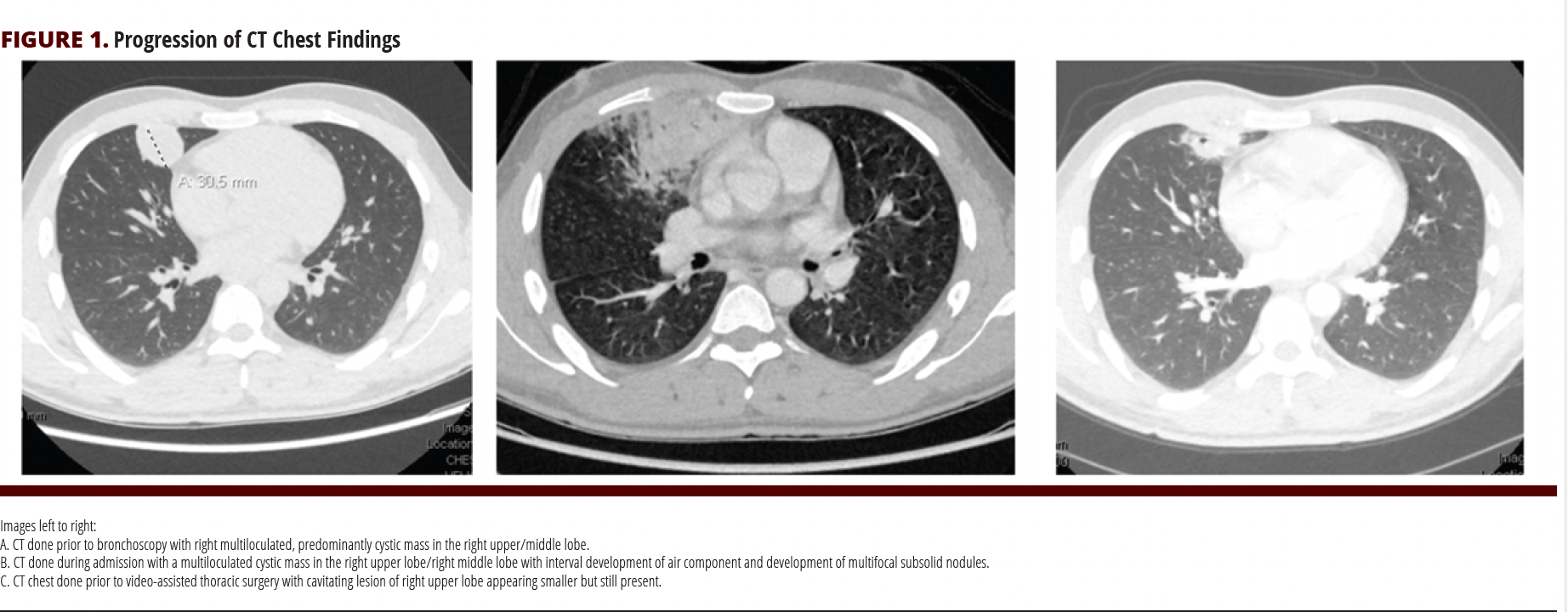
More recently, he was being evaluated as an outpatient for a cough lasting more than 3 years. He was found to have a multiloculated, predominantly cystic mass in his right upper and middle lobes on CT scan of his chest (FIGURE 1A). A week prior to presentation, he had an outpatient diagnostic bronchoscopy for additional work-up of this mass.
EPIDEMIOLOGICAL HISTORY
The patient was born in Afghanistan and lived on a farm with cows, sheep, chicken, cats, and dogs. He worked as a pilot and traveled to numerous countries in Europe, eastern Asia, the Middle East, and South Africa. Three months prior to his current presentation, he moved from Afghanistan to the United States as a refugee and was housed on a military base. Three weeks prior to this presentation, he moved to a hotel where he lived with a roommate. He described himself as active prior to his current health issues. He denies any tobacco, alcohol, or illicit drug use and is not sexually active.
MEDICATIONS
Acetaminophen as needed (not exceeding 3 g/d)
PHYSICAL EXAMINATION
The patient’s vitals were notable for a fever of 101.4 °F, respiratory rate of 24 breaths/ min, and a heart rate of 106 beats/min. He was otherwise hemodynamically stable with an oxygen saturation of 97% on room air. On examination, he was tachypneic and occasionally had a cough with dark brown sputum. He was tachycardic but with a regular rhythm and bilateral wheezing. His abdomen was soft and nontender with a well-healed right upper quadrant scar from his prior surgery.
STUDIES
The patient’s lab work was notable for a white blood cell count of 21.8 B/L (reference range, 4.0-11.0 B/L) with 77.2% neutrophils and 2.5% eosinophils. His lactate was 2.1 mmol/L. The remainder of his complete blood count and comprehensive metabolic panel were within normal limits.
CLINICAL COURSE (SUMMARY OF HOSPITAL COURSE PRIOR TO DIAGNOSIS)
The patient presented to the emergency department and had a chest CT that showed a multiloculated cystic mass in the right upper and right middle lobe (FIGURE 1B). In comparison with his outpatient chest CT from 1 month prior, there was interval development of an air component in addition to numerous new, multifocal, subsolid nodules with adjacent ground glass opacities. A right upper quadrant ultrasound showed no liver cysts. Due to his history of an echinococcal liver cyst, his pulmonary cystic mass and surrounding ground glass opacities were concerning for a ruptured echinococcal cyst possibly with a component of secondary bacterial pneumonia. Ceftriaxone, metronidazole, and albendazole were started. In addition, he was started on nebulized ipratropium and albuterol but did not require epinephrine. He defervesced and his symptoms progressively improved. He continued to have an intermittent cough but with decreased frequency. His sputum production also decreased and changed from foul-smelling, dark-colored sputum to clear sputum. During this hospitalization, the thoracic surgery team did not believe he was an appropriate candidate for surgical resection due to active inflammation and concern for bacterial pneumonia. After 4 days, he was discharged on oral cefuroxime and metronidazole to complete a 2-week course of therapy in addition to oral albendazole, the duration of which would be determined by close outpatient follow-up.
Three weeks after his discharge, he had a repeat CT scan of his chest that showed interval improvement in his multifocal pneumonia with a persistent cavitating lesion of the right upper lobe that appeared smaller compared to prior (FIGURE 1C). He was evaluated by the thoracic surgery team with plans for surgical resection of the remaining cavitary lesion.
DIAGNOSTIC PROCEDURES AND RESULTS
His outpatient bronchoalveolar lavage results prior to his hospitalization had negative fungal, bacterial, and acid-fast bacilli cultures; galactomannan and cytology results were also normal.
During his admission, his work-up was negative for a fourth-generation HIV screen, treponemal antibodies, QuantiFERON-TB Gold, and acute hepatitis panel. His blood and sputum cultures were also negative. An echinococcal IgG enzyme immunoassay and reflexive Western blot were both positive.
After discharge, he underwent a robotic right-sided video-assisted thoracoscopic upper and middle lobe wedge resection. On gross examination, the mass appeared cystic and was completely excised from the lung parenchyma (FIGURE 2). Pathology was suggestive of an echinococcal cyst with chronic pneumonitis and surrounding fibrosis.
TREATMENT AND FOLLOW-UP
Post discharge, he was maintained on albendazole with plans for close follow-up with infectious diseases. In a follow-up, the patient was doing well. His cough had completely resolved. He completed 3 months of oral albendazole postoperatively.

DISCUSSION
Echinococcus is a tapeworm that can be found worldwide.1 There are several species, but disease in humans is caused predominantly by Echinococcus granulosus and Echinococcus multilocularis.2
E granulosus, which can be found in the Middle East, the Mediterranean, South America, China, and sub-Saharan Africa, causes cystic echinococcosis. The life cycle includes definitive hosts (often dogs) and intermediate hosts such as sheep, goats, or swine. Humans do not play a role in the transmission cycle, and so are considered incidental hosts.3 After eggs are ingested by humans, oncospheres hatch from the eggs and can penetrate the intestinal mucosa and travel through the blood or lymphatic system to the liver and other organs. Within days, a cyst can develop.4
Cystic echinococcosis is often asymptomatic until the cyst becomes large enough to cause dysfunction. The most common site of hydatid cysts is the liver, followed by the lungs, although other organs can be involved. If a cyst ruptures, either spontaneously or due to trauma from procedures, then larva can spread from the primary site and form new cysts, which is called secondary echinococcosis.5
The diagnosis of echinococcosis involves a combination of serology and radiographic evidence of a cystic mass in a person with relevant epidemiology. Serologic tests have a high sensitivity and confirmation can be done by demonstrating echinococcal antigens by immunodiffusion procedures or immunoblot assays.5 If serologies cannot be obtained, then aspiration or biopsy of the cyst can be considered, but due to the potential for anaphylaxis and secondary spread of the infection, these interventions are reserved for situations when imaging and serology are nondiagnostic.6,7
Treatment for cystic echinococcosis due to E granulosus depends on the size, stage, and location of the cysts. For small or multiple cysts in several organs, albendazole monotherapy can be used. Surgery is considered if cysts are large; secondarily infected; or located in the brain, lungs, or kidney. A week prior to surgery, albendazole should be given to minimize the risk of secondary echinococcosis and continued for at least 4 weeks.5,8,9 After surgery, recurrence may occur in 2% to 25% of cases.10,11
Another treatment option for cystic echinococcosis is percutaneous aspiration, injection of chemicals, and reaspiration (PAIR). This is less invasive than surgery and has high cure rates. It is indicated for patients who relapse after surgery, fail oral monotherapy, or who decline surgery. Similar to surgery, albendazole should be administered prior to PAIR and continued for at least 4 weeks.10,12,13
The patient in this case report developed secondary echinococcosis of the lung after resection of an echinococcal liver cyst, despite a postoperative course of albendazole. Although he had positive qualitative serologies for echinococcus, speciation could not be performed and pathology did not distinguish between the species. Based on his epidemiology and higher overall prevalence, he presumably had E granulosus. His presentation was likely due to rupture of his pulmonary cyst, and he was successfully treated with preoperative albendazole and antibiotics for secondary bacterial pneumonia, underwent surgical resection, and had a 3-month course of albendazole postoperatively.
References
- Jenkins DJ, Romig T, Thompson RC. Emergence/re-emergence of Echinococcus spp.--a global update. Int J Parasitol. 2005;35(11-12):1205-1219. doi:10.1016/j.ijpara.2005.07.014
- Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev. 2004;17(1):107-135. doi:10.1128/CMR.17.1.107-135.2004
- Moro PL. Epidemiology and control of echinococcus. UpToDate. Updated May 3, 2023. https://www.uptodate.com/contents/epidemiology-and-control-of-echinococcosis
- Parasites – Echinococcosis: Biology. CDC. Updated July 16, 2019. https://www.cdc.gov/parasites/echinococcosis/biology.html
- Parasites – Echinococcosis: Resources for health professionals. CDC. Updated May 21, 2020. https://www.cdc.gov/parasites/echinococcosis/health_professionals/index.html
- Giorgio A, Tarantino L, Francica G, et al. Unilocular hydatid liver cysts: treatment with US-guided, double percutaneous aspiration and alcohol injection. Radiology. 1992;184(3):705-710. doi:10.1148/radiology.184.3.1509053
- Khuroo MS, Dar MY, Yattoo GN, et al. Percutaneous drainage versus albendazole therapy in hepatic hydatidosis: a prospective, randomized study. Gastroenterology. 1993;104(5):1452-1459. doi:10.1016/0016-5085(93)90355-g
- Cobo F, Yarnoz C, Sesma B, et al. Albendazole plus praziquantel versus albendazole alone as a pre-operative treatment in intra-abdominal hydatidosis caused by Echinococcus granulosus. Trop Med Int Health. 1998;3(6):462-466. doi:10.1046/j.1365-3156.1998.00257.x
- Bygott JM, Chiodini PL. Praziquantel: neglected drug? Ineffective treatment? Or therapeutic choice in cystic hydatid disease? Acta Trop. 2009;111(2):95-101. doi:10.1016/j.actatropica.2009.04.006
- Puncture, Aspiration, Injection, Re-Aspiration: an option for the treatment of cystic echinococcosis/WHO Informal Working Group on Echinococcosis. World Health Organization. 2001. https://apps.who.int/iris/handle/10665/67207
- Junghanss T, da Silva AM, Horton J, Chiodini PL, Brunetti E. Clinical management of cystic echinococcosis: state of the art, problems, and perspectives. Am J Trop Med Hyg. 2008;79(3):301-311.
- Brunetti E, Kern P, Vuitton DA; Writing Panel for the WHO-IWGE. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114(1):1-16. doi:10.1016/j.actatropica.2009.11.001
- Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. Bull World Health Organ. 1996;74(3):231-242.

