Ryan K. Shields, PharmD, MS
Articles by Ryan K. Shields, PharmD, MS

Approaches to equitable and responsible antibiotic management
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss the urgent need to ensure equitable access to novel antibiotics, highlighting global and domestic disparities, the vital role of stewardship programs, and the importance of innovative distribution models, international collaboration, and systemic reforms to bring lifesaving treatments to resource-limited settings.

Optimizing formulary decisions and new drug approval through data and team collaboration
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss the complex, systemwide stewardship considerations for incorporating new antibiotics targeting resistant pathogens, emphasizing the need for real-world efficacy data, thoughtful formulary restrictions, and tailored strategies for outpatient use to ensure safe, effective, and sustainable adoption across diverse care settings.

Guiding appropriate use of colistin and polymyxins
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss how regulatory incentives are advancing antimicrobial development, enabling a shift away from older, toxic agents like colistin, while acknowledging that despite the superiority of newer therapies, polymyxins still retain a limited role in rare, highly resistant infections where no better alternatives exist.

Challenges and opportunities in implementing new antibiotics with QIDP and Fast Track status
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss how the clinical use of new antibiotics often extends beyond US Food and Drug Administration (FDA)–approved indications, driven by microbiological activity and clinical judgment, while highlighting the role of regulatory incentives like Qualified Infectious Disease Product (QIDP) in accelerating drug development and the need for careful, collaborative interpretation of limited trial data to ensure responsible off-label use.

Integration of susceptibility testing and local surveillance to inform antibiotic use
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss the challenges of implementing susceptibility testing for new antibiotics, emphasizing the need for close lab-clinician collaboration, streamlined reflex testing protocols, and investment in diagnostic infrastructure to ensure timely and effective treatment of multidrug-resistant infections.

Evidence and trials informing treatment of resistant Gram-negative infections
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss the evolving landscape of novel antibiotic combinations targeting metallo-β-lactamase (MBL)–producing and other multidrug-resistant Gram-negative bacteria, emphasizing promising early data despite limited clinical trials, the complexity of resistance mechanisms, and the potential for these therapies to improve outcomes and shape future treatment strategies.

Strategies for addressing MBL infections with targeted antibiotic combination therapy, and clinical insights from the REVISIT study
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss the innovative use of the aztreonam-avibactam combination to combat complex β-lactamase–mediated resistance, highlighting promising laboratory data, challenges in clinical trial enrollment for resistant infections, and the ongoing need for further research to define its role in treating multidrug-resistant Gram-negative pathogens.

Approaches to challenging cases with limited therapies
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss the real-world challenges of managing infections caused by highly resistant organisms, highlighting the impact of limited access to novel diagnostics and therapeutics, the complexities of outpatient treatment, and the urgent need for broader-spectrum agents and improved delivery methods in resource-constrained settings.

Aligning treatment with risk factors, patient profiles, and MBL status
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss the critical need for a coordinated, multidisciplinary approach to managing infections caused by metallo-β-lactamase (MBL)–producing organisms, emphasizing early identification, containment, careful selection of limited therapeutic options, and stewardship-guided use of novel agents to preserve their long-term effectiveness.

Guiding empirical therapy through patient risk assessment
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss practical strategies for empiric antibiotic selection in the face of rising multidrug resistance, stressing the importance of infection confirmation, patient risk assessment, local resistance data, and stewardship-guided use of newer agents to ensure appropriate and sustainable treatment decisions.

Ryan Shields, PharmD, MS, discusses the challenges of incorporating newer antibiotics for gram-negative infections, how he is using broad-spectrum antimicrobial agents for these infections, and the factors he looks for in considering new agents.

The role of rapid diagnostics and collaboration in antibiotic stewardship
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss the pivotal role of microbiology laboratories and rapid diagnostic technologies in managing multidrug-resistant infections, highlighting their impact on timely treatment, antibiotic stewardship, and the need for interdisciplinary collaboration to effectively interpret and act on resistance data.

Pathogen prevalence, emerging threats, and regional resistance patterns
ByRyan K. Shields, PharmD, MS,Pranita Tamma, MD, MHS,Monica V. Mahoney, PharmD, BCPS, BCIDP, FCCP, FIDSA, FIDP, FMSHP,Rodney E. Rohde, PhD, MS, SM(ASCP)CM, SVCM, MBCM, FACSc; and Ryan P. McNamara, PhD Panelists discuss emerging therapies for multidrug-resistant Gram-negative pathogens, focusing on the rising threat of antimicrobial resistance, evolving resistance mechanisms like extended-spectrum β-lactamases (ESBLs) and New Delhi metallo-β-lactamases (NDMs), regional variability in pathogen prevalence, and the clinical implications for treatment in inpatient and outpatient settings.
Resistance against this pathogen with β-lactamase medications
can vary according to geographic region.
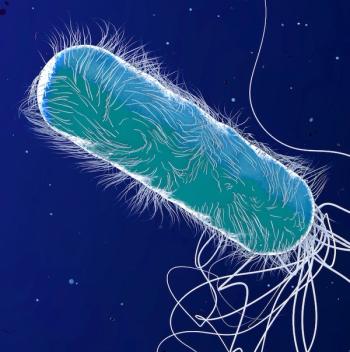
Rates of hospital-onset multidrug-resistant P aeruginosa infections have increased significantly in recent years.

Carbapenem-resistant Enterobacterales present considerable treatment challenges. Recent cumulative evidence supports preference for therapies.
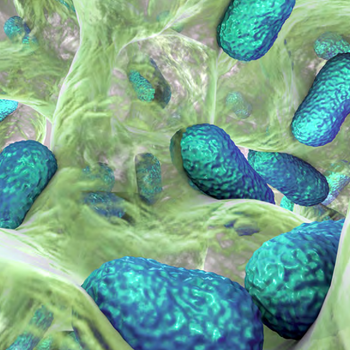
Recent study results show promising new modalities.

This approach can help with clinical outcomes and mortality, but resistance is not as well defined.

Ceftazidime-avibactam is a novel treatment for CRE infections, but reports of resistance are increasing.