
Prof. Andrea Endimiani, MD, PhD, from the Institute of Infectious Diseases at the University of Bern, Switzerland, explains which pathogens are most affected by the colistin resistant mcr-1 gene.

Prof. Andrea Endimiani, MD, PhD, from the Institute of Infectious Diseases at the University of Bern, Switzerland, explains which pathogens are most affected by the colistin resistant mcr-1 gene.

John Mohr, PharmD, president and founder of Medical Affairs Strategic Solutions, LLC, explains the current state of the antimicrobial pipeline.

Monica Mahoney, PharmD, BCPS-AQ ID, clinical pharmacy coordinator of infectious diseases at Beth Israel Deaconess Medical Center, explains the antimicrobial considerations that are specific to the solid organ transplant population.

Emily Heil, PharmD, BCPS-AQ ID, from the University of Maryland School of Pharmacy, discusses the concerns of antibiotic use in agriculture.

Jason C. Gallagher, PharmD, president, Society of Infectious Diseases Pharmacists, explains if we know how the case of mcr-1 E. coli superbug was contracted.

New research suggests that modernized phages therapy may be useful in extending the lifespan of currently available antibiotics and reducing the incidence of antibiotic-resistant infections.

Marion A. Kainer, MD, MPH, FRACP, FSHEA, Director of Healthcare Associated Infection and Antimicrobial Resistance Program, Tennessee Department of Health, discusses some of the key points to aid in the fight against healthcare associated infections, nationwide.

Jason C. Gallagher, PharmD, President, Society of Infectious Diseases Pharmacists describes the recent case of an antibiotic resistant “superbug” in Pennsylvania.

With reports in the mainstream media prophesizing doom with regard to the issue of antimicrobial resistance, a committee formed by the British government has released a report designed to properly contextualize the crisis and develop recommendations for addressing it.

A recent review article on the status of vaccines in development for healthcare associated infections (HAIs) provides both an in-depth discussion of their urgent need, as well as their potential for success.

Researchers from the department of pathology at the Beth Israel Deaconess Medical Center in Boston developed and validated a high-throughput screen (HTS) that could detect antimicrobial agents with the ability to restore carbapenem susceptibility to resistant strains, as well as those that target CRE directly.

For patients who suffer from certain uncomplicated infections such as, sinusitis, bronchitis, and uncomplicated urinary tract infections, the health risks associated with fluoroquinolone far outweigh the benefits.

Older antibiotic agents show decreased potency due to overuse and the subsequent emergence of drug-resistant bacteria. This antimicrobial resistance has been predicted to have enormous consequences for human health, necessitating the development of new agents in the ongoing war between humans and the germs that attack us.

Antibiotic-resistant pathogens continue to make the management of some bacterial infections a significant clinical challenge.
Adding to the troubling data worldwide on antibiotic resistance, researchers have found that even trace concentrations of antibiotics, such as those found in sewage, are sufficient for bacteria to maintain resistance to most broad-spectrum agents.
Two new inhibitory compounds—named KKL-10 and KKL-40—could hold the key to preventing the proliferation of the highly virulent bacterium Francisella tularensis, according to a recent study.
On April 18, 2016, the director-general of the World Health Organization, Margaret Chan, OBE, JP, discussed antimicrobial resistance at a United Nations briefing in New York.

On March 8, 2016, researchers at the Ulsan National Institute of Science and Technology reported the development of an antibacterial fabric that inhibits the growth of bacteria, including antibiotic-resistant bacteria.

Dorothy McCoy, PharmD, explains what patients in the hospital should do if they have concerns about their medications.

US hospitals have made significant reductions in the incidence of hospital-acquired infections (HAIs) over the past decade, a new report from the Centers for Disease Control and Prevention (CDC) has revealed.
The Centers for Disease Control and Prevention believes far too many Americans are exposed to "dangerous, drug-resistant bacteria" in hospitals and other healthcare settings.

Jason C. Gallagher, PharmD explains the most important thing healthcare practitioners should keep in mind about antimicrobial stewardship.
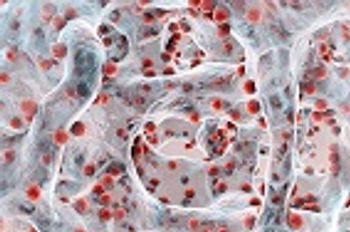
Researchers have discovered a new class of chemical compounds that work to inhibit biofilm formation, thereby identifying a potential new therapeutic target for the treatment of infections caused by Acinetobacter baumannii.

A recent article endeavors to draw new-- and perhaps increased-- attention to the issue of neurologic side effects associated with antibiotic use in hospitalized patients.

Jason C. Gallagher, PharmD explains what healthcare providers can do to help address antimicrobial resistance.