
Coronavirus / COVID
Latest News
Latest Videos

CME Content
More News

Viruses and other concerns within medicine are being overlooked; health care preparedness must address these potential crises.
Social media platforms, public health agencies, and communities must join forces to stop the rapid spread of false information.
The strain, Eris (EG5), is from the Omicron lineage, and the expectations are the newest vaccines will protect against it, and other variants from the same family.

Surveillance data such as hospitalizations and wastewater metrics provide real COVID-19 prevalence numbers, but do we need to do more to be prepared ahead of another potential health crisis?

A new study confirms this form of surveillance to collect metrics for SARS-CoV-2 to understand infection prevalence on a bigger scale.
A new study demonstrated Moderna having a greater efficacy and slightly less adverse event profile in this patient population vs the Pfizer-BioNTech vaccine.

New report published this week shows the decrease over the last 2 reportable years.

Patients with cancer, cancer survivors, and matched controls maintained immunity against severe COVID-19 for at least 5 months after a third or fourth vaccine dose.

Workplace exposure and living conditions were associated with higher COVID-19 risk, while previous infection, age 65 or older, and Black/African American race were correlated with lower COVID-19 rates.

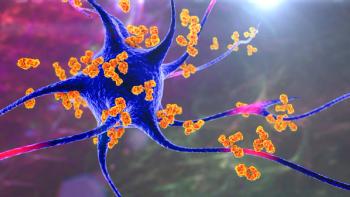
This study found a substantial increase in Alzheimer's-related deaths during the initial year of the pandemic due to limited access to healthcare, social isolation, and disrupted care routines. However, the second year brought positive developments with prevention strategies and vaccinations, leading to a substantial decline in excess deaths.

More symptoms, older age, and longer hospitalization time increased the risk of post-COVID-19 conditions (long COVID) in children.
Neuropilin-1 enables COVID-19 to enter human cardiomyocytes, accounting for increased proteases activity and apoptotic markers that lead to cell damage and apoptosis.

This study analyzed 81 communities in Los Angeles and found that once vaccines became widely available, there was no significant difference in COVID-19 incidence between communities of varying income levels.
Though rare, Guillain-Barré syndrome can occur after vaccination. Did Pfizer-BioNTech, Moderna, or Janssen COVID-19 vaccination increase the risk of Guillain-Barré syndrome?

This examination of vaccine introductions worldwide reveals significant gaps in access, especially in low-income countries.
Researchers investigated abatacept, cenicriviroc, and infliximab, but found that these medications did not significantly impact the time to recovery from COVID-19 pneumonia compared to placebo.

These study findings highlight higher in-hospital mortality rates for patients with preventable conditions during COVID-19.

The findings showed that heterologous vaccination, or mixing different vaccines, was safe and effective, with the Novavax vaccine (NVX-CoV2373) providing enhanced protection against the Omicron variant.

This variant, which is an ancestor of Omicron, is an emerging variant that is being seen most frequently in Utah, California, and New York State.

A small study explored the connection between Postural Orthostatic Tachycardia Syndrome (POTS) and the COVID-19 condition.

Patients who perceived brain fog within 4 weeks of COVID-19 infection were twice as likely to report symptoms of long COVID than patients without cognitive deficits.

There was a lower risk of Omicron infection for each 10-fold increase in preinfection IgG, and for each 2-fold increase in neutralizing antibody titers.

In Indiana, COVID-19 patients with chronic obstructive pulmonary disease, cardiovascular disease, and type 2 diabetes had significantly higher mortality rates than COVID-19 patients without these comorbidities.
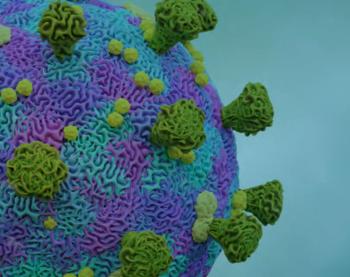
The strain, identified as EU11, accounts for 1.7% of cases nationwide in the United States.

Non-enveloped viruses were resistant to all types of wash products and duration tested, including synthetic soaps, such as the ones typically used in hospitals.











































































































































