C. Difficile
Latest News
Latest Videos

CME Content
More News

Highlights from the morning session of the C Diff Foundation Conference included data about Pfizer's investigational vaccine, insights about Seres Therapeutics microbiome therapeutic, and a look at CDI incidence rates around COVID-19.

Curtis Donskey, MD, discussed his efforts to encourage C. diff patients and providers to do their part to reduce infection and reinoculation.
The development of these programs are being looked at for private practices in the community settings to try to create better prescribing practices and avoid the potential progression to health care associated infections.

The organization is hosting its 9th Annual International C Diff Conference and Health EXPO on Thursday and Friday this week. The conference is virtual and free to the public.

A new study in Israel supports the use of a shorter course of antibiotics for the treatment of complicated urinary tract infection in recipients of kidney transplants.

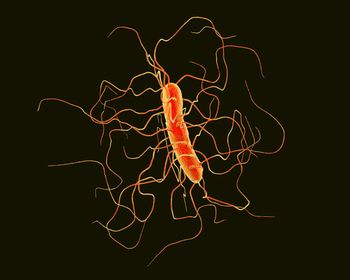
Incidences of Clostridioides difficile infection have risen in recent years, and understanding risk factors can help practitioners address associated mortality, morbidity and health care costs.


Higher use of 7 major antibiotics in hospitals is corelated with higher rates of Clostridioides difficile infection.

CDI remains an urgent public health threat and continues to be the most frequent cause of diarrhea among hospitalized patients and overall hospital-acquired infection in the United States.

A global study of C. difficile isolates worldwide found a very high prevalence of the bacteria on shoe soles.

With fecal microbiota transplants (FMT) becoming a potential emerging therapy for these patients, here are some aspects to consider when treating.
Purified nisin is effective at killing Clostridioides difficile, a recent ex vivo study demonstrated, opening up the potential to use the bacteriocin as a treatment.


What are the efforts being made with antibiotic stewardship and treatments, and what areas in clinical care do medical professionals want to see improvements.

The company’s RBX2660, administered as a single dose, demonstrated superiority over standard of care for reducing Clostridioides difficile infection (CDI) recurrence.

This event will be a free, virtual event in July with expert speakers and survivors.

Investigators apply guidelines into practical management strategies.

The organizations set out 3 recommendations for initial and recurrent C diff treatment.

During the COVID-19 surge last year, the federal government stopped the required reporting on healthcare-associated infections (HAI) thus leaving an absence of data and important information on HAI. One study examined the effect the initial pandemic surge had on Clostridioides Difficile infection (CDI) in one hospital.

An assessment of the frontline agents show similarities infection cure and recurrence rates at 30 days.

Ferring Pharmaceuticals and Rebiotix reported results from a trial on their therapy, RBX2660, which shows promise as a Clostridioides difficile infection (CDI) treatment.

A study looked at hospital admissions of Medicare patients and saw a large percentage of recurrent Clostridioides difficile infections (rCDI) as the primary diagnosis.

An effort to increase stewardship showed that 5-day and 10-day prescription stop dates for antibiotics did little to influence actual therapy length and outcomes.

A large retrospective analysis of Medicare patients offers a glimpse of the incidence rates of this patient population and the burdens associated with it.

A meta-analysis suggest the 2 first-line C diff therapies provide similar outcomes, yet differ in recurrent infection risk.