Advances in the CDI Treatment Landscape
Experts discuss new and emerging treatments the management of CDI, highlighting the phase 3 trials for SER 109.
Episodes in this series

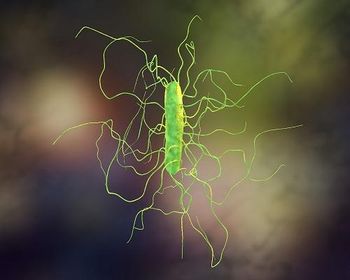
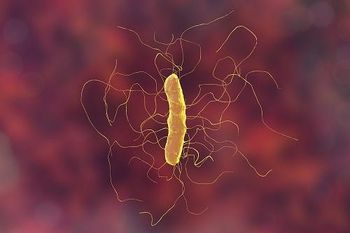
Stuart Johnson, MD: Thank you. Candace, what are some other advances in the landscape for treating CDI, and particularly, recurrent CDI?
Candace Cotto, RN: Right now they're also looking at SER-109, which was a clinical trial with an oral fecal transplant. It prevented recurrent CDI in about 88% of patients vs the placebo arm, which was only about 60%. The safety profile was the same in both arms. And the only differences between RBX2660 and SER-109 is that the SER-109 is only replacing the Firmicutes, where the Rebiotix RBX2660 was replacing more than just the Firmicutes.
Stuart Johnson, MD: That's an interesting question. The SER-109 product was basically alcohol-shocked stool specimens from donors also screened, but again, left with spores of primarily Firmicutes and missing the component Bacteroides. So, it did seem to work well in this clinical trial and, in fact, was stratified by both antibiotic treatment and by age, and it's for all 3 of those stratifications or both of those stratifications it seemed to be effective. Candace, thank you for mentioning SER-109, this new FMT product that's likely going to be approved in the near future. What about other advances in therapy? Anything out there that anyone is aware of?
Joseph Reilly, PharmD, BS, BCGP: Besides the product we had just mentioned, I would imagine there may be some products in development aimed at correcting dysbiosis. And what health care professionals need to ask themselves now is, when we have these products available that go at the cause of recurrent C diff by correcting dysbiosis, that's the problem, how do we ignore them? In other words, are we going to wait for the third episode of C diff, or if we see somebody that had C diff, it was their first time and they were very sick and hospitalized and traumatized by this episode, how do we ignore an available treatment that's out there that can be a game-changer for that patient? So the guidelines are one thing and a lot of the guidelines from IDSA [Infectious Diseases Society of America] and ACG [American College of Gastroenterology] are also based on FMT [fecal microbiota transplant] from the older data involving a bowel prep and colonoscopy and propofol. This is a big procedure that's invasive. Now that we have other products out there, it should change the way we view treatment in these patients.
Stuart Johnson, MD: Yes, I agree. The landscape has changed now with at least 1 FDA-approved product that addresses this dysbiosis. In general, people would like to see a more defined microbiome. Way back in the '80s, there was a report by this Danish group where they took a collection of 10 different bacteria that they grew up in the lab and that somewhat represented in their mind a healthy microbiome and administered it to patients. The key is still out there, or the key component of the microbiome that needs replacement or that is important placement, is still an open question. But it'd be nice to eventually get to a point where we know exactly what we're giving the patients and can define it in a molecular or microbiome aspect, if you will. And people have also done filtrates from patients' stool samples, and that seems to work, too. So, what exactly is the key component of the microbiome that needs replacement? In the future, if we talk 10 years from now, maybe we'll have a more defined bacterial composition. What about drugs? Is there anything out there? To refresh everyone's memory, FMT is an adjunctive treatment. It's not treatment per se of C difficile. But we're still going to need drugs for treatment.
Andrew Skinner, MD: And so fidaxomicin was the last FDA-approved antibiotic that we have for C difficile at this point, which was approved back in 2011. We have had some couple of newer things going through the clinical trials at this point right now, so ridinilazole is one of the more selective therapies as well. But the future of that is still in question at this point as well. We don't know if it's going to meet their goals that they were looking for it to be approved for the treatment of C difficile. And then we also have –
Stuart Johnson, MD: I’ll say it. Ibezapolstat. This is another antibiotic treatment that's been proposed for C difficile. It involves DNA polymerase 3. It's an interesting component. It's had a phase 1 trial that was very nice, but not controlled, and they're in the middle of a phase 2 trial right now just to compare it to vancomycin. So, we may have another antibiotic option. As far as ridinilazole goes, this was a victim of the COVID-19 pandemic, if you will. They had 2 large multinational phase 3 trials that were stopped midway during the study because of difficulty in enrollment and they put the data together and submitted a statement, if you will, but I don't think it's been officially reported yet, the outcomes. So, don't know if it's dead yet, but it's possible. As you mentioned, Andrew, that it looks to be a more narrow spectrum antibiotic. So, both ridinilazole and ibezapolstat might be available in the near future.
Joseph Reilly, PharmD, BS, BCGP: It's interesting, you say a narrow spectrum antibiotic, and when fidaxomicin became available, what was appealing about it is that it had a narrow spectrum, and it could spare some of those good bacteria. So once again, we're back at dysbiosis, which seems to me to be the biggest problem. Currently we have effective antibiotics for the treatment of active C diff. Vanco still works. Metronidazole still works in many patients. And fidaxomicin is effective. So, the problem with C diff, the way I see it, is the recurrences in these patients. Now that we have an available product and more on the way, it'll be beneficial for this population, in particular, and definitely beneficial from a hospital perspective in decreasing these numbers that are readmitted again and again and again.
Andrew Skinner, MD: One of the bigger roles for the more narrow spectrum antibiotics, and it's why fidaxomicin was pushed up towards the top of line for initial courses as well. So that's where it's going to have the biggest bang for its buck as well, is that if we can limit the dysbiosis associated even with vancomycin and that initial treatment course and we go to fidaxomicin and then the next one is, let's say, antibiotic x; that's the next one that's finally approved, are they causing less and less dysbiosis and after that initial episode we're seeing fewer recurrence at that point. I agree that these newer therapies that are affecting the microbiota are going to be very critical when we start running into recurrent C difficile infections.
Transcript edited for clarity
Newsletter
Stay ahead of emerging infectious disease threats with expert insights and breaking research. Subscribe now to get updates delivered straight to your inbox.